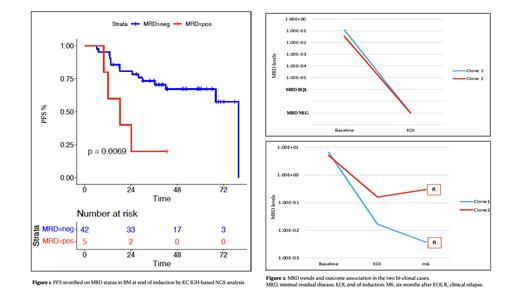
Background. Despite durable clinical responses achieved by chemo-immunotherapy in follicular lymphoma (FL) patients, most of them eventually relapse. Actually, minimal residual disease (MRD) analysis based on the detection of BCL2::IGH rearrangement by PCR is the most widely used and standardized approach, able to early identify patients at high risk of disease reappearance. Nevertheless, this tool fails the molecular marker definition in up to 45% of cases, hampering the disease monitoring in a large group of patients. In the last decade, the continuous improvement of next-generation sequencing (NGS) techniques allowed to introduce these novel tools for MRD monitoring in some hematologic diseases, as acute lymphoblastic leukemia and multiple myeloma, thus reducing PCR limitations and increasing the number of patients eligible for MRD. Nonetheless, applications of NGS tools for MRD detection in FL are still scant. Aims. Therefore, we tested the feasibility of the EuroClonality (EC) IGH-based NGS approach [Brüggeman, Leukemia 2019] to identify novel molecular markers suitable for MRD monitoring in the context of the large prospective trial “FOLL12” (EudraCT: 2012-003170-60) by the Fondazione Italiana Linfomi (FIL), where 57% of patients were already studied for MRD by classic PCR methods targeting the BCL2::IGH rearrangement.[Luminari, JCO2022] Methods. Advanced FL patients received upfront treatment with either R-CHOP or BR, followed by a combined PET/MRD response-based maintenance with rituximab. Bone marrow (BM) samples were centralized to the FIL MRD Network for standardized MRD analysis. Baseline gDNA of “no marker” patients was screened by IGH-based NGS using EC-IGH two-steps PCR approach in the EuroMRD certified lab of Torino university; then MRD was monitored in those patients harboring a IGH clonal marker at baseline by one step EC-IGH method. The identification of baseline clonotypes and MRD clones was performed by ARRest/Interrogate tool. Results. 343/786 enrolled patients (43%) lacked a conventional BCL2::IGH marker and 161/343 (47%) showed morphologic BM lymphoma infiltration: of these, 124 (77%) had an available BM baseline sample for IGH screening and were thus included in the analysis. Overall, IGH clonotypes suitable as novel molecular markers were identified in 75/124 patients (60%), of which 73 monoclonal and 2 biclonal. Of this series, 47 patients had centralized a BM sample for MRD analysis at end of induction. Median age of this subset was 59 years (33-81), 53% were female, all were Ann Arbor stage IV, 34% were FLIPI intermediate and 43% high risk, respectively. Moreover, 56% received R-CHOP and 44% BR as induction treatment, resulting in a 79% CR rate and 89% MRD negativity rate (in line with the results of the general trial population). PFS at 3 years for this series was 69%: however, the 5 patients who scored MRD positive (MRD+) showed statistically significant worse PFS at 3 years than MRD negative cases (22% vs 73%, respectively, p=0.0069, Figure 1). Notably, 4 out of 5 MRD+ patients experienced POD24. Focusing on biclonal cases, one presented superimposable MRD trends between clones (both achieving MRD negativity), while in the other both clones remained MRD positive but showing one Log difference between them. Interestingly, only one of the two clones showed a MRD increase in the following timepoint (6 months after end of induction), heralding the clinical relapse subsequently occurred at month 12 (Figure 2). On the other hand, no IGH clonotype was identified in the first 17 patients who were screened for a novel MRD marker despite the absence of BM infiltration. Conclusions. The first data on the large-scale application of NGS-based marker screening tools in FL patients lacking a conventional BCL2::IGH marker for MRD enrolled in a prospective clinical trial showed that the EC IGH-based NGS approach was able to provide a new molecular marker in 60% of patients with evidence of BM infiltration (that means about the 28% of “no marker” FL patients); importantly, this approach was predictive of worse PFS for MRD+ cases. Overall, these data are promising for the wide employment of novel, effective MRD monitoring tools, able to recover more than one fourth of FL patients lacking a conventional molecular marker and so, by combining conventional and NGS-based techniques, potentially rising the percentage of MRD evaluable cases up to at least 70% cases.
Disclosures
Genuardi:Werfen: Honoraria. Galimberti:Abbvie, Janssen, Novartis, Roche, Jazz, Astra Zeneca, Pfizer, Incyte: Speakers Bureau. Del Giudice:Astra-zeneca, Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees. Ladetto:Novartis: Honoraria. Luminari:Incute: Membership on an entity's Board of Directors or advisory committees; Regeneron: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BMS: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Beigene: Membership on an entity's Board of Directors or advisory committees; Jannsen: Membership on an entity's Board of Directors or advisory committees; ROCHE: Membership on an entity's Board of Directors or advisory committees. Ferrero:Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; EUSA Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Abbvie: Consultancy; Sandoz: Consultancy; Beigene: Research Funding; Morphosys: Research Funding; Incyte: Membership on an entity's Board of Directors or advisory committees; Clinigen: Membership on an entity's Board of Directors or advisory committees; Servier: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Gentili: Speakers Bureau; Italfarmaco: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal